Understanding the product and the physiology behind it
This comprehensive review explores the safety profile of a popular vaping brand and explains how it may affect cardiovascular measures, with a special focus on the intersection of IBvape|e cigarettes and blood pressure. The aim is to provide vapers, clinicians, and curious readers with an evidence-informed synthesis that balances product-specific considerations, general e-cigarette science, and practical harm-reduction guidance. The analysis avoids hyperbole, prioritizes mechanisms, regulatory context, and actionable recommendations for safer device use and health monitoring.
What is this device category and what does “IBvape” represent?
Products in this category vary from simple refillable pen systems to modular, high-power devices. For the purposes of risk appraisal, it is helpful to think in layers: device hardware (battery, heater, design), e-liquid composition (nicotine concentration, solvents, flavorants), user behavior (puff topography, frequency), and biological susceptibility (age, cardiovascular history). When readers search for IBvape|e cigarettes and blood pressure they often seek clarity on whether a specific brand alters blood pressure acutely or chronically. This review unpacks the evidence and separates what we know from what remains uncertain.
Key components that influence cardiovascular response
- Nicotine: a well-known stimulant that elevates heart rate and transiently increases blood pressure by activating the sympathetic nervous system.
- Propylene glycol (PG) and vegetable glycerin (VG): solvents that generally have low systemic toxicity but can produce irritant aerosols; their thermal decomposition can create small amounts of aldehydes under certain conditions.
- Flavoring chemicals: a heterogeneous group; some are considered safe for ingestion but lack inhalation safety data. Certain compounds have been implicated in respiratory inflammation which can indirectly influence cardiovascular stress.
- Ultrafine particles and metals: aerosols may deliver particulate matter that affects endothelial function and vascular tone.
How these components can change arterial pressure
The acute blood pressure response to inhaled aerosols is primarily driven by nicotine-induced catecholamine release, vasoconstriction, and increased cardiac output. Secondary pathways include reflex autonomic responses to inhalation, oxidative stress from particles and reactive chemicals, and inflammatory signaling that can alter vascular reactivity. The net effect depends on nicotine dose, rate of absorption, baseline cardiovascular health, and device characteristics that affect aerosol yield.
What the research literature says about e-cigarettes and blood pressure
Several observational and interventional studies have examined short-term changes in systolic and diastolic blood pressure after use of various e-cigarette devices. Many acute challenge studies document modest elevations in heart rate and systolic pressure immediately after vaping sessions, especially with nicotine-containing liquids. Long-term epidemiological data are less consistent: cross-sectional surveys sometimes report associations between current vaping and higher self-reported hypertension, but causality is challenging to infer due to confounding by prior smoking, dual use, and lifestyle factors. The keyword cluster IBvape|e cigarettes and blood pressure often appears in consumer searches where short-term effects are of greatest concern.
Clinical trials and quality of evidence
Randomized controlled trials comparing nicotine replacement therapies, combustible cigarettes, and e-cigarette use have primarily focused on smoking cessation outcomes and respiratory measures. Cardiovascular endpoints beyond immediate hemodynamic measures are less frequently assessed. Where trials exist, they suggest that switching completely from combustible cigarettes to e-cigarettes reduces exposure to many combustion-derived toxicants, which could lower long-term cardiovascular risk; however, persistent nicotine exposure via vaping may continue to affect blood pressure and heart rate. Thus, for smokers switching to IBvape|e cigarettes and blood pressure-relevant outcomes, the decision involves weighing reduced exposure to smoke toxicants against continued nicotine-driven sympathetic stimulation.
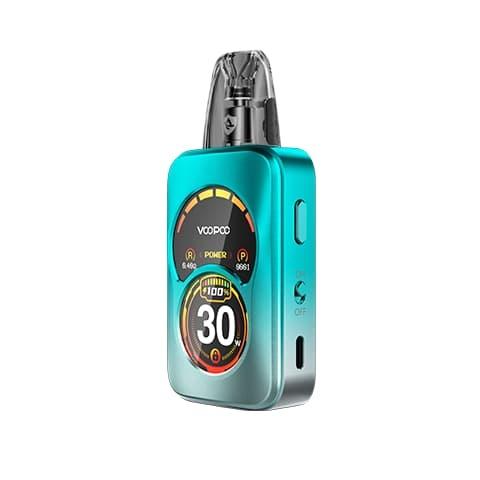
Device- and product-specific safety considerations
The design and maintenance of devices influence aerosol chemistry. High coil temperatures, dry puffs, or misuse can generate more thermal breakdown products. Battery safety is a separate but important concern for physical injury rather than cardiovascular risk. For vapers concerned about blood pressure changes, product selection can mitigate risk: preferring lower nicotine concentrations, using regulated devices that prevent excessive coil temperatures, and avoiding aftermarket modifications that increase aerosol yield dramatically.
Tips to reduce cardiovascular impact while vaping
- Choose the lowest effective nicotine concentration to control cravings, recognizing that higher nicotine leads to stronger hemodynamic effects.
- Avoid deep, rapid inhalation patterns that increase systemic nicotine absorption; practice paced use if monitoring blood pressure changes.
- Use devices with temperature control or wattage limits to reduce formation of potentially pro-oxidant byproducts.
- Maintain devices cleanly—replace coils and wicks per manufacturer guidance to avoid overheating and off-flavors that may signal thermal degradation.
- Steer clear of unregulated or counterfeit products, which may contain unexpected ingredients or inconsistent nicotine delivery.


Who should be most cautious?
People with pre-existing hypertension, coronary artery disease, heart failure, diabetes with vascular complications, the elderly, and pregnant people should approach any nicotine-containing product with caution. For these groups, the acute pressor effects of nicotine can be clinically relevant. Clinicians should inquire specifically about vaping habits when assessing cardiovascular risk and discuss nicotine cessation strategies tailored to the individual.
Monitoring and clinical recommendations
Practical steps for vapers and healthcare providers who are tracking cardiovascular response include home blood pressure monitoring, timing measurements relative to vaping sessions (e.g., baseline resting measure and repeat 15–30 minutes post-use), and tracking heart rate. Establishing a baseline while abstaining for a period can clarify whether chronic vaping is associated with persistently higher readings. For individuals switching from cigarettes to e-cigarettes, repeated measures may reveal improvement in long-term vascular markers despite transient nicotine-related spikes.
Regulatory context and product quality
Regulatory frameworks differ globally and affect product safety. Where quality standards are enforced, manufacturers are required to test for contaminants, label nicotine content accurately, and adhere to battery and electrical safety norms. In markets with limited oversight, consumers face greater uncertainty about ingredient lists and device integrity. Searching for “IBvape|e cigarettes and blood pressure” often leads users to community forums—these can be useful for user experiences but lack the rigor of controlled data.
Behavioral strategies and cessation options
For vapers seeking to lower cardiovascular risk, consider a structured cessation plan: behavioral counseling, pharmacotherapies (prescription nicotine replacement, varenicline, bupropion), and step-down strategies that reduce nicotine gradually. If vaping is being used as a smoking cessation tool, the ideal outcome from a cardiovascular standpoint is complete abstinence from nicotine over time. Clinicians should tailor recommendations to patient preference and readiness, balancing harm reduction with ultimate cessation goals.
When acute care is needed
If a vaper experiences severe chest pain, syncope, acute neurological deficit, or markedly elevated blood pressure readings (e.g., systolic >180 mmHg or diastolic >120 mmHg with symptoms), seek immediate medical attention. Mild to moderate elevations in blood pressure after vaping are often transient, but persistent or symptomatic changes require clinical evaluation.
Real-world user guidance
Practical harm-reduction suggestions for everyday use include: keeping nicotine strengths consistent to avoid accidental overdosing, logging device settings and e-liquid brands to identify patterns linked to symptoms, staying hydrated, and avoiding vaping in combination with stimulants like cocaine or high-dose caffeine which compound sympathetic effects. For vapers monitoring their blood pressure, avoid measuring immediately after caffeine or exercise to isolate vaping-specific effects.
Summary of evidence and balanced takeaways
The current body of evidence indicates that nicotine-containing e-cigarettes can produce short-term increases in heart rate and blood pressure; the magnitude depends on dose, device, and user behavior. Switching from combustible cigarettes to e-cigarettes may reduce long-term exposure to many toxicants associated with cardiovascular disease, but vaping with nicotine is not risk-free. For consumers concerned about IBvape|e cigarettes and blood pressure, the most impactful actions are to reduce or eliminate nicotine exposure, choose regulated products, and engage with healthcare providers to monitor cardiovascular health.
Research gaps and future directions
High-priority research questions include: long-term cardiovascular outcomes among exclusive vapers who previously smoked versus those who never smoked, the role of specific flavoring chemicals in vascular inflammation, dose–response relationships for nicotine delivered via modern devices, and the effects of dual use (cigarettes plus e-cigarettes). Improved device and aerosol characterization in studies will enhance the relevance of findings to brands and product families in real-world use.
Practical checklist for vapers worried about blood pressure
- Measure resting blood pressure weekly and log symptoms.
- Try reducing nicotine stepwise while monitoring cravings and blood pressure.
- Use regulated devices with safety features and avoid temperature extremes.
- Consult a clinician if you have cardiovascular disease or persistent hypertension.
- Report any alarming symptoms such as chest pain or fainting to emergency services.

In short, the intersection of IBvape|e cigarettes and blood pressure is best understood as a balance between reduced exposure to smoke toxicants (if switching from combustible tobacco) and the persistent hemodynamic effects of nicotine. Individual risk varies; informed choices and medical oversight improve outcomes.
Quick resources and references
For further reading, consult systematic reviews on e-cigarette cardiovascular effects, guidelines from national cardiology societies, and product stewardship pages from reputable manufacturers. Community resources may offer practical tips but should not replace clinical advice. Users can search clinical trial registries and pubmed-indexed reviews for the latest evidence.
Closing practical advice
Vapers seeking to minimize cardiovascular impact should favor reduced nicotine exposure, choose quality-controlled products, and track blood pressure. Health professionals should ask explicitly about vaping habits and consider short- and long-term monitoring when relevant. Ultimately, cessation remains the most effective way to eliminate nicotine-related blood pressure effects.
If you want brand-specific testing data for a particular device or e-liquid, request lab reports from manufacturers or seek independent testing organizations that publish detailed aerosol chemistry and heavy metal analysis; transparency in labeling and third-party verification are hallmarks of higher-quality products. The keyword IBvape|e cigarettes and blood pressure can guide your queries, but prioritize peer-reviewed data and regulatory disclosures over anecdote.
This content is educational in nature and does not substitute for medical advice. If you have a cardiac condition, are pregnant, or are taking medications for hypertension, consult your healthcare provider before using any nicotine product.
FAQ
Does vaping raise blood pressure more than smoking?
Short answer: not necessarily in the short term. Combustible cigarettes deliver a complex mix of combustion products that contribute to long-term cardiovascular risk; e-cigarettes typically reduce exposure to many combustion-related toxins but still deliver nicotine which raises blood pressure acutely. The net long-term cardiovascular risk depends on complete switching versus dual use and cumulative exposure.
Can IBvape specifically be linked to hypertension?
There is no robust public evidence that any single brand alone causes chronic hypertension beyond nicotine’s well-established physiological effects. Product quality, nicotine concentration, and user patterns matter more than brand name in determining cardiovascular responses.
How can I check if my vaping device is safe for blood pressure concerns?
Check for regulated device features, accurate nicotine labeling, third-party lab testing of e-liquids, and manufacturer transparency. Monitor your blood pressure before and after use to detect any individual sensitivity.